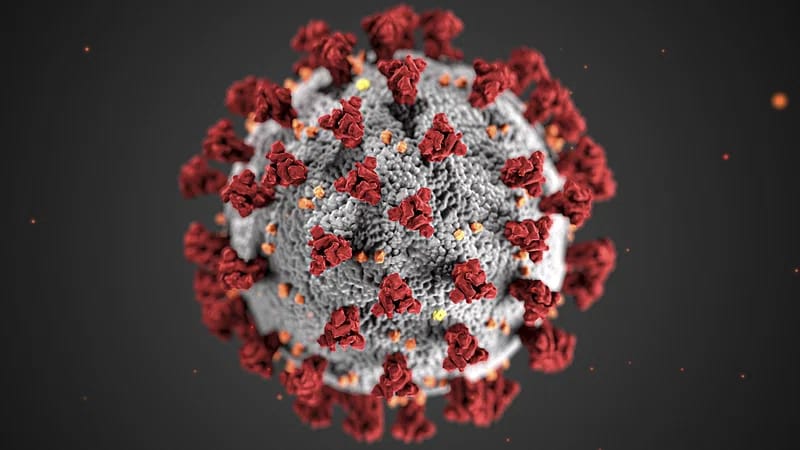
Human Metapneumovirus (HMPV virus) is a respiratory pathogen that has garnered attention in recent years due to its significant impact on public health. Belonging to the Pneumoviridae family, HMPV virus is closely related to Respiratory Syncytial Virus (RSV) and primarily affects the respiratory system. Discovered in 2001, this virus is now recognized as a major cause of acute respiratory infections (ARIs) worldwide, particularly in young children, older adults, and individuals with weakened immune systems. Understanding the HMPV virus is crucial for developing effective strategies to combat its spread and mitigate its effects on vulnerable populations.
Table of Contents
ToggleWhat is HMPV?
HMPV virus is a negative-sense, single-stranded RNA virus that is thought to have been circulating in human populations for decades before its discovery. Retrospective studies have detected evidence of HMPV infections dating back to the 1950s. The virus is divided into two main genetic lineages, A and B, each further subdivided into sub-lineages (A1, A2, B1, and B2). These genetic variations allow the virus to adapt and evade host immune responses, contributing to its persistence and seasonal outbreaks.
The Lifecycle and Characteristics of HMPV virus
HMPV virus attaches to the epithelial cells of the respiratory tract using its surface glycoproteins, namely the fusion (F) protein and attachment (G) protein. Once inside the host cell, the virus replicates its RNA genome, producing new viral particles that infect neighboring cells. This process triggers an inflammatory response, leading to the respiratory symptoms commonly associated with HMPV infections.
Symptoms of HMPV Infection
Common Symptoms
HMPV infections typically present with symptoms similar to those of other respiratory viruses, making it difficult to diagnose without specific testing. Common symptoms include:
-Runny nose
-Cough
-Fever
-Sore throat
-Congestion
In most healthy individuals, these symptoms are mild and resolve on their own within a week or two.
Severe Symptoms in Vulnerable Populations
In high-risk groups, such as infants, the elderly, and those with underlying health conditions, HMPV can cause severe respiratory illnesses, including:
Bronchiolitis
Pneumonia
Exacerbation of asthma or chronic obstructive pulmonary disease (COPD)
Respiratory failure in extreme cases
How Does HMPV Spread?
HMPV is highly contagious and spreads through several routes:
- Respiratory droplets: When an infected person coughs or sneezes, viral particles are released into the air.
- Direct contact: Touching surfaces contaminated with the virus and then touching the face (eyes, nose, or mouth).
- Close contact: Prolonged exposure to an infected individual, especially in crowded or enclosed spaces.
Incubation Period
The incubation period for HMPV typically ranges from 3 to 6 days, during which the infected person may already be contagious.
Diagnosis of HMPV
Diagnosing HMPV can be challenging due to its similarity to other respiratory viruses like RSV and influenza. However, specific diagnostic methods include:
- RT-PCR Testing
Real-time polymerase chain reaction (RT-PCR) is the most reliable method for detecting HMPV RNA in respiratory specimens. It is highly sensitive and specific, making it the gold standard for HMPV diagnosis.
- Antigen Detection
Immunofluorescence assays can detect HMPV antigens in respiratory samples, providing a quicker, though less sensitive, diagnostic option.
- Serology
Serological tests measure antibodies against HMPV in blood samples, useful for retrospective studies but not for acute diagnosis.
Prevention of HMPV
Preventing HMPV requires a combination of personal hygiene practices and community-wide measures.
Personal Hygiene Practices
Frequent handwashing with soap and water for at least 20 seconds.
Avoiding close contact with individuals showing symptoms of respiratory infections.
Disinfecting surfaces that are frequently touched, such as doorknobs, phones, and countertops.
Vaccination Research
While no vaccine for HMPV is currently available, researchers are actively working on developing vaccines and antiviral treatments. Advances in mRNA technology, similar to those used in COVID-19 vaccines, hold promise for future HMPV prevention strategies.
Treatment of HMPV
Currently, there is no specific antiviral treatment for HMPV. Management of the virus focuses on relieving symptoms and supporting the immune system.
Supportive Care
Hydration: Drinking plenty of fluids to prevent dehydration.
Rest: Allowing the body to recover.
Medications: Over-the-counter medications like acetaminophen or ibuprofen to reduce fever and alleviate pain.
Hospitalization
In severe cases, especially among high-risk groups, hospitalization may be required for oxygen therapy or mechanical ventilation.
The Impact of HMPV on Global Health
HMPV is a significant contributor to the global burden of respiratory infections, particularly in resource-limited settings where access to diagnostic and treatment facilities is limited. Studies estimate that HMPV accounts for 5-10% of acute respiratory infections in children under five years of age. Its impact is compounded during seasonal outbreaks, placing additional strain on healthcare systems.
Economic Burden
The economic cost of HMPV includes:
Medical expenses: Doctor visits, hospital stays, and medications.
Lost productivity: Parents missing work to care for sick children and individuals being unable to work during illness.
HMPV in the Era of COVID-19
The COVID-19 pandemic has highlighted the importance of monitoring and controlling respiratory viruses like HMPV. Increased adoption of preventive measures, such as mask-wearing and social distancing, has inadvertently reduced the spread of HMPV and other respiratory viruses. However, as these measures are relaxed, a resurgence of HMPV cases has been observed in some regions.
Future Directions in HMPV Research
- Vaccine Development
The development of a safe and effective vaccine against HMPV is a top priority for researchers. Advances in virology and immunology are paving the way for innovative vaccine platforms.
- Antiviral Therapies
Exploring antiviral drugs that target specific stages of the HMPV lifecycle could provide new treatment options.
- Improved Diagnostics
The integration of point-of-care testing and molecular diagnostics in healthcare settings can enhance the detection and management of HMPV.
Conclusion
Human Metapneumovirus (HMPV) is an often-overlooked yet significant respiratory pathogen that poses a considerable threat to vulnerable populations worldwide. By understanding its characteristics, transmission routes, and impact, we can implement effective prevention and management strategies. As research continues to advance, the development of vaccines and antiviral therapies offers hope for reducing the burden of HMPV. Public awareness and global cooperation will play a crucial role in combating this virus and safeguarding public health.
Human Metapneumovirus (HMPV) is a respiratory virus that primarily affects the lungs and airways, causing symptoms similar to the flu or common cold. In 2025, it has gained significant attention due to recent outbreaks, advances in diagnostic methods, and its potential to impact vulnerable populations like children and the elderly. Improved understanding of its transmission and prevention has become a global healthcare priority.
The symptoms of HMPV include:
Fever
Cough
Shortness of breath
Nasal congestion
Sore throat
Wheezing (in severe cases)
Infants, older adults, and immunocompromised individuals are at a higher risk of severe complications, such as pneumonia and bronchiolitis.
HMPV is transmitted through respiratory droplets when an infected person coughs or sneezes. It can also spread via contact with contaminated surfaces or close personal interactions. To prevent infection:
Practice regular hand hygiene.
Wear masks in crowded spaces.
Avoid close contact with infected individuals.
Disinfect frequently touched surfaces.
Stay updated on healthcare guidelines and vaccinations, if available.
As of 2025, there is no specific antiviral treatment for HMPV. Management typically involves supportive care, such as hydration, fever control, and oxygen therapy for severe cases. However, significant progress has been made in vaccine development, with clinical trials underway. Consult a healthcare professional for the latest updates on treatments and prevention.
